We’ve spent years working with electronic health records, and the sheer volume of healthcare data we generate daily amazes us. Hospitals like Cleveland Clinic or Mayo Clinic produce around 137 terabytes of patient information every day. That’s enough data to fill thousands of smartphones!
Electronic health record systems have revolutionized how healthcare providers manage patient care in the United States. Yet, many professionals in the healthcare industry struggle to understand the fundamental difference between structured and unstructured data in their EMR platforms. These two types of data are the yin and yang of medical information management.
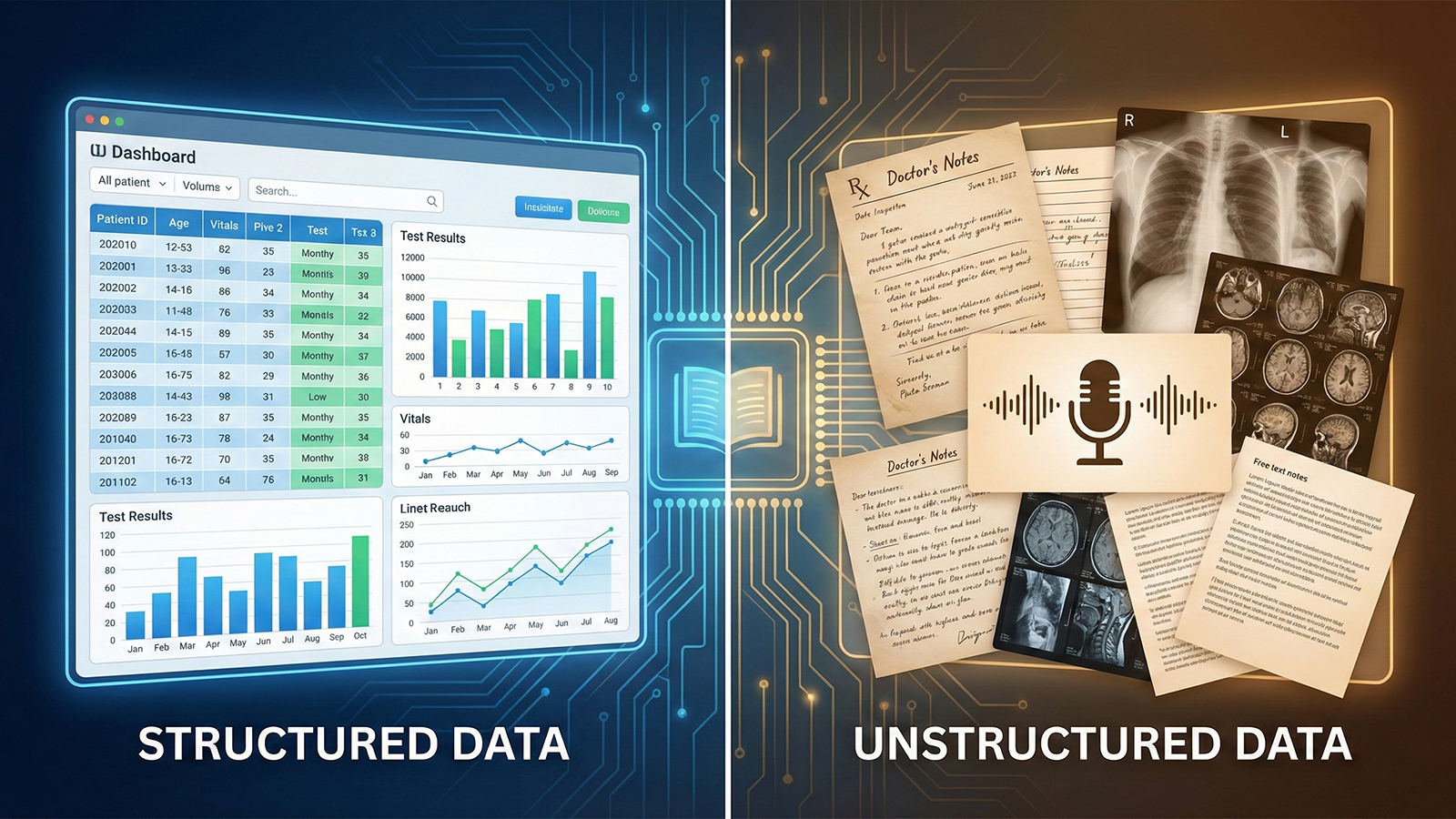
Structured data is like a neat filing cabinet in your office – everything is labeled and ready to find. Lab results from Quest Diagnostics, vital signs recorded by Phillips monitors, and medication lists from CVS Health all fit into predefined fields. On the other hand, unstructured data is the doctor’s handwritten notes, radiology reports from GE Healthcare imaging systems, and discharge summaries that tell the patient’s story in narrative form.
The healthcare data explosion isn’t slowing down. With genetic testing companies like 23andMe entering the clinical space and wearables from Apple Watch to Fitbit feeding patient-generated health data into healthcare systems, we’re seeing a 47% yearly increase in data generation. This tsunami of information presents both incredible opportunities and significant challenges for electronic health providers nationwide.
Key Takeaways
- Healthcare facilities generate approximately 137 terabytes of data daily through EMR systems
- Structured data includes organized, searchable information in predefined fields like lab results and vital signs
- Unstructured data encompasses narrative text, clinical notes, and imaging reports that require different processing methods
- Healthcare data generation increases by 47% annually due to medical devices and patient-generated health information
- Understanding both data types is essential for improving patient care quality and clinical decision-making
- The average hospital manages roughly 50 petabytes of data yearly, twice the Library of Congress collection
What Is Structured Data in Healthcare EMR Systems
Structured data in healthcare follows a predefined data model. This makes patient information easy to search, analyze, and share. It’s like filling out a form where each piece of patient data goes into its designated box. This format allows your healthcare organization to quickly access vital information when making critical decisions about patient care.
Using structured data in EMR systems organizes information into specific fields within data stores. Each data type has its place – from blood pressure readings to medication dosages. This is different from unstructured notes where doctors write free-form observations. Structured data typically appears as dropdown menus, checkboxes, and numerical fields that staff can quickly complete during patient visits.
Key Components of Structured Data
The foundation of structured data offers several essential elements that every healthcare organization relies on:
- Demographics (name, date of birth, insurance ID)
- Vital signs (blood pressure, temperature, weight)
- Laboratory results with numerical values
- ICD-10 diagnostic codes
- Medication lists with exact dosages
- Billing codes and procedure records
Benefits for Clinical Decision-Making
Structured data vs unstructured text shows clear advantages in clinical settings. Physicians can instantly spot medication conflicts, track treatment progress, and identify patterns across patient populations. When data is stored in standardized formats like SNOMED CT or LOINC codes, different systems can communicate seamlessly. This reduces medical errors and improves care coordination.
Common Examples in Patient Records
| Data Category | Examples of Structured Fields | Storage Format |
|---|---|---|
| Patient Demographics | SSN, DOB, Gender, Address | Alphanumeric fields |
| Clinical Measurements | BP: 120/80, Glucose: 95 mg/dL | Numerical values with units |
| Medications | Metformin 500mg, twice daily | Coded drug names, dosages |
| Diagnoses | E11.9 (Type 2 Diabetes) | ICD-10 codes |

Unstructured Data: The Hidden Wealth in Electronic Health Records
Structured data fits neatly into predefined fields, but unstructured data tells a richer story. It’s like the difference between checking boxes on a form versus having a real conversation with your doctor. Unstructured data doesn’t follow rigid rules – it flows naturally, capturing the nuances that checkboxes miss.
Types of Unstructured Clinical Information
Examples of unstructured data fill every corner of modern healthcare. Progress notes capture a physician’s observations in their own words. Discharge summaries tell the complete story of a hospital stay. Radiology reports describe what doctors see in medical images beyond simple measurements.
Nursing staff document patient interactions in free-form text. Physical therapists write detailed assessments of movement and recovery. Even patients contribute through personal health narratives and symptom descriptions. This unstructured format preserves context that structured fields would lose.
Why Unstructured Data Matters for Patient Care
Unstructured data provides insights that diagnostic codes can’t capture. When physicians document severity levels or note subtle symptoms, they’re creating valuable clinical context. Social determinants of health – housing situations, family support, transportation challenges – live in these notes. Unstructured data offers a complete picture of patient wellness beyond lab results.
Volume and Storage Challenges
Working with unstructured imaging data presents unique challenges. A single chest X-ray requires 15 megabytes. A 3D mammogram needs 300 megabytes. Digital pathology files can reach 3 gigabytes each. Organizations must harness unstructured data while managing explosive growth. Transforming unstructured information into actionable insights requires sophisticated storage strategies and retention policies.
Critical Differences Between Structured and Unstructured Data
The distinction between structured and unstructured data in healthcare information significantly impacts how data scientists and data engineers handle patient records. The structured vs unstructured data formats present unique hurdles for clinical teams dealing with big data in EMR systems.
Structured and unstructured data have distinct roles in data science. Structured data, such as lab values and vital signs, is easily organized in databases. On the other hand, unstructured data, like clinical notes and imaging reports, uncovers deeper patient narratives. Semi-structured data, a blend of both, offers a middle ground.
| Data Characteristic | Structured Data | Unstructured Data | Semi-Structured Data |
|---|---|---|---|
| Storage Format | Relational databases | Document stores | NoSQL databases |
| Analysis Speed | Immediate processing | Requires NLP tools | Moderate processing |
| Common Healthcare Examples | ICD-10 codes, lab results | Physician notes, radiology reports | HL7 messages, XML files |
| Volume in EMRs | 20% of healthcare data | 80% of healthcare data | Variable percentage |
Understanding these differences is key to making data actionable. Studies indicate that specific data from unstructured sources can meet 59% of lymphocytic leukemia trial criteria and 77% of prostate cancer eligibility needs. Data engineers must navigate the complexities of both data formats to aid in clinical decision-making.

Integrating Both Data Types for Better Healthcare Outcomes
Healthcare professionals gain powerful insights by combining structured and unstructured patient data. Structured data provides quantifiable metrics like lab values and vital signs. On the other hand, unstructured data offers critical context through physician notes and patient narratives. This integration transforms healthcare data into actionable intelligence, improving treatment decisions.
Natural Language Processing Applications
Natural language processing (NLP) changes how clinical teams extract meaning from text-based records. Machine learning algorithms scan through discharge summaries, progress notes, and consultation reports. They identify symptoms, medications, and diagnoses that might be missed in structured fields.
The Mayo Clinic’s cTAKES system is a prime example, processing millions of clinical documents. It extracts temporal features present in 40% of clinical trial criteria. These artificial intelligence tools help clinicians spot patterns in patient complaints and treatment responses.
Clinical Decision Support Systems
Clinical decision support systems combine both data types to alert providers about risks. When a physician prescribes medication, these systems analyze structured allergy lists and unstructured nursing notes. This dual approach helps prevent adverse events by catching subtle warnings that single data sources might miss.
Real-time alerts have reduced medication errors by up to 55% in hospitals using integrated systems. This shows the importance of combining data for patient safety.
Risk Stratification and Predictive Analytics
Predictive analytics models perform best when analyzing complete patient stories. Risk stratification tools examine structured demographics and lab results. They also mine clinical notes for social determinants and behavioral patterns.
This holistic view is critical in identifying patients likely to need readmission within 30 days. It enables care teams to intervene proactively with targeted support programs.

Overcoming Data Management Challenges in Modern Healthcare
Healthcare organizations face immense pressure to manage the vast amounts of data daily. They must ensure data security and facilitate seamless data exchange. This requires a balance between technical innovation and strict regulatory compliance to safeguard patient information.
Data Privacy and Security Considerations
Patient data contains sensitive information that must be protected. Healthcare facilities employ encryption, access controls, and audit trails to prevent breaches. HIPAA compliance is key, driving organizations to establish protocols for data privacy across all systems.
Interoperability Standards and Protocols
Diverse healthcare systems struggle with data exchange due to different formats and standards. Fast Healthcare Interoperability Resources (FHIR) offers a framework for sharing data between platforms. Organizations adopt standards like HL7 and DICOM to facilitate communication across various data sets and clinical applications.
Learn More: Mediportal’s Industry-Leading Interoperability Solution
Storage Optimization Strategies
Healthcare demands smart storage optimization due to the sheer volume of data. Cloud migration helps manage data across multiple locations, reducing costs. IT teams classify data workloads by frequency, moving less-used records to lower-cost storage tiers.
The Role of AI in Data Normalization
AI normalization transforms unstructured clinical notes into standardized formats for analysis. Machine learning algorithms process data from various sources, mapping it to coding systems like ICD-10 and SNOMED. This automated process efficiently handles massive data sets, surpassing manual processing capabilities.

How Mediportal’s EMR Helps With Data For Better Health Outcomes
Healthcare organizations in the United States are overwhelmed by data. Each facility generates about 50 petabytes of data annually. This creates both opportunities and challenges for healthcare professionals aiming to enhance patient care. Mediportal tackles this issue by turning raw data into actionable insights, driving better healthcare outcomes.
Our EMR software bridges the gap between structured metrics and unstructured clinical narratives. This integration is highly valuable in specialties like mental health EMRs. Here, patient stories are as important as numerical assessments. Healthcare stakeholders using Mediportal gain a complete view of each patient’s journey. This enables personalized treatment plans that meet individual needs.
The platform organizes data on patient histories, treatment responses, and population health trends. Modern healthcare demands such sophistication. Mediportal’s system processes numerous data points, from lab results to physician notes. It creates detailed patient profiles that support clinical decision-making.
Healthcare applications within Mediportal transform scattered information into cohesive insights. The software helps identify patterns across patient populations, predict complications, and allocate resources efficiently. This approach has helped facilities across the United States reduce readmission rates and improve treatment adherence.
By unifying diverse data streams, Mediportal empowers healthcare professionals. It allows them to focus on delivering exceptional patient care through informed, data-driven decisions.
Conclusion
The healthcare industry is at a turning point, where both structured and unstructured information hold immense power for change. Electronic health records now collect a wide range of data, from coded diagnoses to detailed physician notes. This rich data set enables healthcare providers to make more informed decisions and tailor treatments that are effective.
Big data in healthcare has evolved beyond mere storage. It’s now about transforming patient data into actionable insights. Institutions like Cleveland Clinic and Mayo Clinic are already leveraging AI to analyze this data, leading to enhanced diagnosis and treatment outcomes. The approach is to start with specific goals, focusing on particular areas of data analysis.
The path forward is both clear and challenging. Healthcare providers must have the right tools to handle diverse data types while ensuring patient data security. The American Hospital Association emphasizes the need for hospitals to become data-driven to better serve their communities. By effectively combining structured and unstructured data, healthcare systems can unlock the full promise of modern medicine. This includes delivering better care, making diagnoses faster, and fostering healthier populations.