Legacy EMR systems are a major obstacle for healthcare organizations in the United States. If you manage IT or clinical administration in healthcare, you’re familiar with the frustration of outdated platforms. These systems resist integration with newer technology.
Working with numerous healthcare facilities has shown me the importance of seamless data exchange. Yet, many are stuck with electronic medical record systems from decades ago. These interoperability barriers are not just technical issues. They also affect patient safety and your organization’s financial stability.
Statistics paint a grim picture. Between 2003 and 2008, over 30% of hospitals changed vendors, leading to high costs and long transition times. Legacy systems hinder healthcare teams’ ability to coordinate care across the ecosystem.
That’s where specialized solutions come in. Mediportal is a leading provider of Healthcare Interoperability Software. It helps organizations overcome seemingly insurmountable technical hurdles. This guide will show how interoperability is essential for your daily operations and how to overcome these challenges.
Key Takeaways
- Legacy EMR systems create significant barriers to data exchange between healthcare organizations
- Over 30% of hospitals switched EMR vendors between 2003-2008, highlighting widespread dissatisfaction
- System transitions are expensive, time-consuming, and require substantial personnel resources
- Modern healthcare demands seamless interoperability across fragmented care environments
- Specialized healthcare interoperability software like Mediportal bridges gaps between incompatible systems
- Technical barriers affect both patient safety outcomes and organizational financial performance
Understanding Legacy EMR Systems in the Modern Healthcare Ecosystem
The backbone of many healthcare organizations today isn’t cutting-edge technology—it’s legacy electronic health record systems. These platforms, once revolutionary, now struggle to meet modern healthcare demands. They power everything from small clinics to mid-sized hospitals across the United States, managing patient data but creating interoperability challenges.
Dealing with outdated software is complex. We face an entire ecosystem of healthcare technology built for a different time. Many healthcare organizations are caught between maintaining what works and embracing future needs.
At Mediportal, we understand these challenges. We work with healthcare providers across the United States who face this dilemma daily. Let’s explore what defines legacy systems, their prevalence, and why healthcare organizations stay with them despite limitations.
Learn More: What Is Interoperability in Healthcare? A Beginner’s Guide
What Defines a Legacy EMR System
Legacy EMR systems are not just “old software.” They’re EHR systems designed before interoperability standards became the norm. These platforms run on outdated architectures, not designed for seamless data exchange.
Legacy systems are like older homes with 1970s electrical wiring. Sure, the lights work, but modern devices don’t fit. Legacy ehr systems handle basic documentation but struggle with sharing information across systems.
Here’s what characterizes legacy electronic health record platforms:
- Built 10 to 20 years ago on outdated programming languages and database structures
- Lacks modern APIs and standardized protocols necessary for seamless data exchange
- Requires manual data entry or custom interfaces to communicate with other platforms
- Operates on proprietary data formats that don’t align with current interoperability standards
- Struggles to integrate with newer healthcare technology like patient portals or mobile health apps
The technical limitations are significant. Legacy systems lack interoperability features that modern ehr systems include. When different healthcare organizations use different systems, the gap becomes a chasm.
The Widespread Use of Outdated Electronic Health Record Technology
Many healthcare organizations rely on legacy platforms due to competing priorities. They know their systems aren’t ideal but face insurmountable barriers to change.
The financial investment in current systems is substantial. Hospitals invested millions in ehr vendor partnerships years ago. Leadership questions the need for more spending when what they have works.
Functionality isn’t the same as effectiveness. Electronic medical record keeping has evolved. Many healthcare organizations use systems not designed for this expanded role.
Here’s what keeps healthcare organizations tethered to legacy ehr systems:
- Embedded operational workflows: Staff have been trained on these systems, often for years. Clinical workflows are built around specific features and quirks. Changing the system means rebuilding processes from the ground up.
- Data migration complexity: Moving years or decades of patient records from one system to another isn’t like transferring files between folders. Legacy data structures often don’t map cleanly to modern formats.
- Integration with existing technology: The legacy EHR might be connected to dozens of other systems used by the organization—lab equipment, billing platforms, scheduling tools. Each connection needs to be rebuilt or replaced.
- Resource constraints: Healthcare providers face constant pressure on budgets and staffing. Taking on a major system replacement while maintaining patient care quality requires resources many organizations simply don’t have.
The systems used today weren’t designed for the level of integration now required. Yet, many healthcare organizations run multiple systems that refuse to communicate effectively with each other or with external providers.
This is where Mediportal makes a difference. We understand that replacing systems overnight without disrupting patient care is impossible. Our approach focuses on building bridges between legacy ehr systems and modern healthcare technology, creating pathways for data exchange that work with your existing infrastructure.
The challenge isn’t just technical—it’s organizational, financial, and deeply human. But understanding why many healthcare organizations rely on legacy systems is the first step toward finding practical solutions that don’t require betting the entire organization on a risky, expensive replacement project.

Key Challenges of Interoperability Facing Healthcare Organizations
Healthcare IT leaders often discuss the same challenges of interoperability in healthcare. These are not minor issues but major obstacles that hinder data exchange and patient care quality. The main challenge lies in connecting fragmented systems, which were never designed for interoperability.
Understanding each barrier is key to developing targeted solutions. This approach is better than simply throwing technology at the problem. Let’s explore the four major categories of interoperability issues faced by healthcare organizations in the United States.
| Challenge Category | Primary Impact | Affected Systems | Implementation Difficulty |
|---|---|---|---|
| Outdated Data Standards | Communication breakdowns between systems | Legacy EHR, lab systems, imaging platforms | High – requires complete protocol updates |
| Data Silos | Fragmented patient information across departments | Clinical, administrative, pharmacy, radiology | Medium – needs unified data architecture |
| Vendor Lock-In | Proprietary formats blocking data transfer | Multi-vendor environments | Very High – contractual and technical barriers |
| Missing Interoperability Features | No native connectivity capabilities | Pre-2010 legacy platforms | Very High – may require complete replacement |
Outdated Data Standards and Communication Protocols
Legacy platforms built with proprietary methods are a major interoperability challenge. These systems are difficult to connect to external healthcare components.
Many older systems lack support for modern standards like Fast Healthcare Interoperability Resources (FHIR). This barrier to interoperability is like trying to have a detailed medical conversation between two people who speak different languages.
Even with attempts to bridge these gaps, the lack of standardized protocols leads to custom integration work for every connection point. This is expensive, time-consuming, and fragile, as one system update can break everything.
Data Silos and Fragmented Patient Information
Poor interoperability leads to patient data being isolated across your organization. Radiology images, lab results, pharmacy data, and clinical documentation are stored in different systems.
This fragmentation is a significant challenge for healthcare organizations. Accessing a patient’s complete health information requires manually accessing multiple systems, which is time-consuming and dangerous.
Data silos slow down workflows and directly impact patient safety. Critical health information trapped in separate systems leads to decisions based on incomplete information, increasing the risk of medical errors.
The average cost of a healthcare data breach is $7.42 million, the highest among all industries. These breaches often exploit gaps between siloed systems, where security oversight is inconsistent.
Vendor-Specific Barriers to Data Exchange
Vendor-specific barriers are a major frustration. Many EHR systems use proprietary formats that create artificial walls around health information. Even when vendors claim support for interoperability standards, the implementation varies significantly, making reliable data exchange a massive undertaking.
These challenges exist partly because vendors have historically benefited from “lock-in” strategies. Making it difficult for you to leave their ecosystem or connect to competitors keeps you as a captive customer.
The variation problem is insidious. Systems might use different terms for the same data, like “BP” versus “blood pressure.” Without semantic standardization, sharing patient data across systems becomes an exercise in translation that strips away critical context.
Context surrounding clinical data often disappears during transfer between vendor systems. This leaves providers with decontextualized facts that are difficult to interpret for clinical decision-making.
Lack of Built-In Interoperability Features in Legacy Platforms
The lack of built-in interoperability features in legacy platforms is a significant barrier. These systems were not designed for the seamless connectivity modern healthcare demands.
They lack APIs, standardized interfaces, and architectural flexibility needed for interoperability. This creates technical challenges that affect clinical workflows and billing processes.
Data quality problems compound these technical limitations. Issues like duplicate patient records, inconsistent formatting, and missing units of measurement compromise the reliability of shared information. Semantic interoperability relies on data quality for information to be accurate, complete, and interpretable.
Dealing with these EHR interoperability challenges can feel overwhelming. You can’t afford to rip and replace everything, but you also can’t continue operating with systems that prevent effective data exchange.
That’s where specialized solutions come in. At Mediportal, we’ve built our platform to address these technical challenges facing healthcare organizations across the United States. Our approach bridges the gaps created by legacy systems, providing the middleware and integration capabilities needed for a connected healthcare ecosystem. We do this without requiring you to abandon your existing technology investments entirely.
Learn More: Common Interoperability Challenges in Small Practices
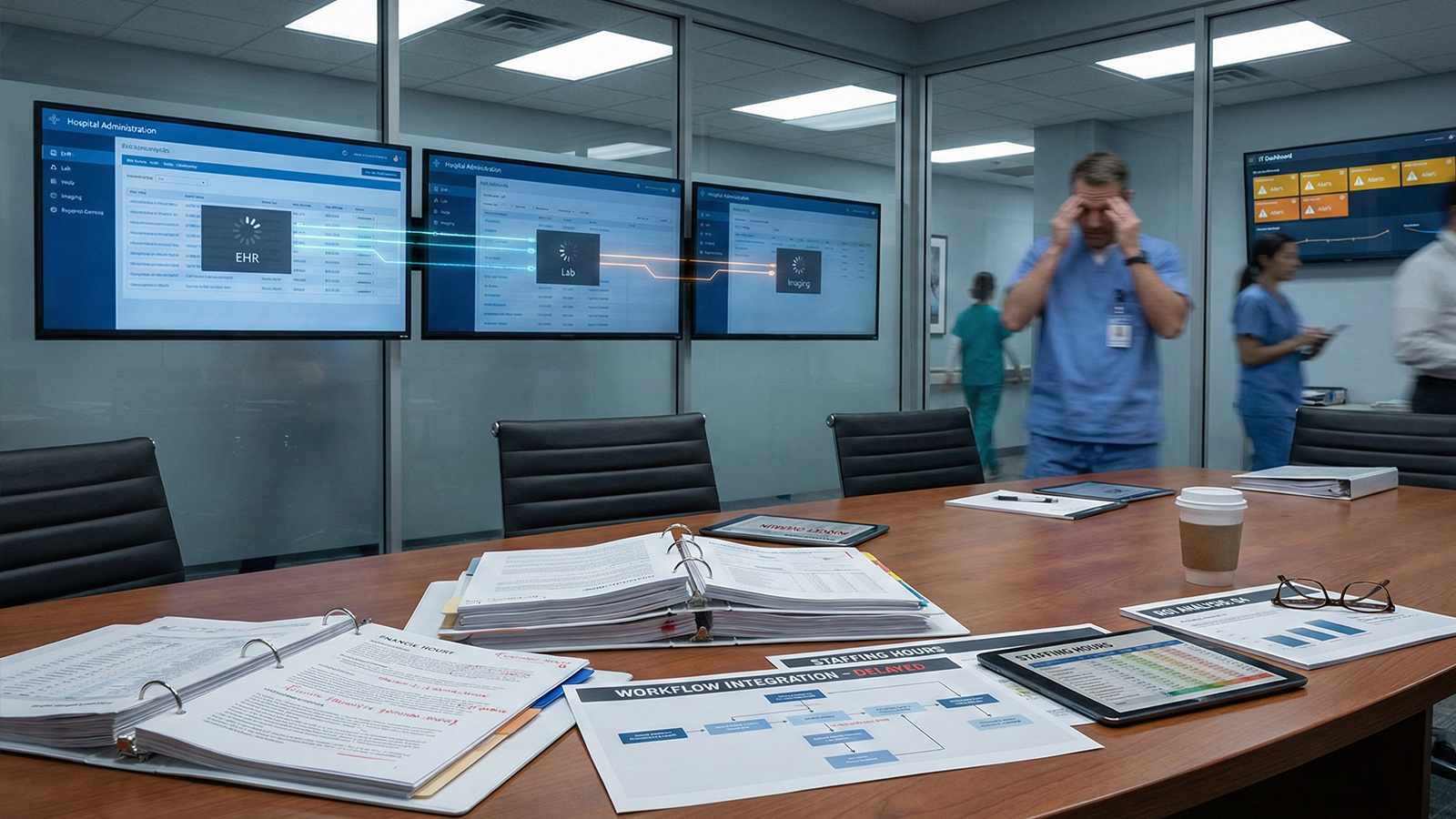
Organizational, Financial, and Human Challenges to Achieving Interoperability
Achieving interoperability is more than just solving technical puzzles. It involves navigating a complex landscape of financial constraints, human resistance, and operational realities. While data standards and protocols pose formidable obstacles, organizational barriers can be equally challenging. Healthcare organizations face pressures from budget committees demanding ROI justification, clinical staff resisting workflow changes, and executives balancing innovation with operational stability.
These non-technical factors often determine whether interoperability initiatives succeed or stall indefinitely. Understanding these challenges is the first step toward overcoming them with practical, realistic strategies.
The Significant Financial Burden of System Modernization
The massive financial investment required to improve interoperability across legacy systems is a significant challenge. When healthcare organizations decide to modernize, they face expenses that extend far beyond the initial software purchase.
Large healthcare systems can expect total costs ranging from $250 million to over $1 billion for system transitions. This includes the new system purchase, implementation, training, data migration, and ongoing maintenance.
Consulting fees alone can run 1.5 to 10 times your normal analyst rates. If you decide to maintain your legacy system alongside a new platform during transition, you’re adding hundreds of thousands annually just for dual-system maintenance.
The hidden costs hit even harder. Physicians get pulled away from revenue-generating patient care to serve on implementation committees. Nurses spend valuable time in training sessions instead of at the bedside. Your IT department works overtime, often without additional compensation.
These expenses don’t appear on vendor proposals, but they significantly impact your bottom line. Personnel shifted to implementation duties, lost revenue from reduced clinical capacity, and opportunity costs from delayed projects all add up quickly.
Change Management and Healthcare Staff Resistance
The human side of interoperability often determines success or failure, regardless of budget size. Healthcare staff—particular overworked clinicians—frequently view new systems with justified skepticism. They’ve experienced “improvements” that created more work, not less.
Achieving full interoperability requires buy-in from the people using these systems daily. That means addressing real concerns about workflow disruption, steep learning curves, and whether the change will genuinely help healthcare delivery or just add administrative burden.
Clinician resistance isn’t irrational—it’s based on experience. When interoperability requires logging into multiple systems, navigating unfamiliar interfaces, or spending precious minutes hunting for information that used to be readily available, pushback is inevitable.
Communication fatigue is real. Healthcare staff already juggle numerous alerts, messages, and system notifications. Adding another layer of technology without streamlining workflows creates resistance that can derail even well-funded initiatives.
Effective change management isn’t just about training sessions and go-live support. It’s about genuinely understanding how these systems impact daily work and designing solutions that support interoperability while respecting clinical workflows. When healthcare leaders ignore this human element, projects fail despite technical excellence.
Resource Constraints That Healthcare Organizations Face
Here’s a sobering reality: 47% of healthcare organizations ranked IT staffing shortages in their top three challenges in 2025. You’re being asked to achieve true interoperability while operating with understaffed IT departments already juggling security threats, system maintenance, user support, and countless other priorities.
Interoperability requires specialized expertise—professionals who understand integration engines, data standards like HL7 and FHIR, healthcare workflows, and regulatory requirements. These unicorn professionals are in extremely short supply across the healthcare industry.
Healthcare organizations need to either pay premium rates for consultants or invest time and money upskilling existing staff. Both options strain already-tight budgets and timelines. The numerous challenges this creates cascade through your organization, slowing projects and inflating costs.
| Resource Challenge | Impact on Interoperability | Typical Timeline Delay | Cost Implication |
|---|---|---|---|
| IT Staffing Shortages | Delayed implementation and reduced project scope | 3-6 months | 15-25% budget increase for consultants |
| Lack of Integration Specialists | Poor system connections and data mapping errors | 4-8 months | High consultant fees or failed integrations |
| Limited Clinical Champion Availability | Workflow misalignment and low adoption rates | 2-5 months | Rework costs and extended training periods |
| Competing IT Priorities | Fragmented focus and incomplete implementations | 6-12 months | Ongoing dual-system maintenance costs |
Clinical staff must also invest significant time learning new systems and workflows. This takes them away from patient care during already demanding workdays. Investing in interoperability means temporarily reducing clinical capacity, which many organizations simply can’t afford.
Balancing Patient Care Continuity with System Upgrades
Unlike upgrading your smartphone, healthcare systems can’t just go offline for maintenance. Healthcare depends on 24/7 access to critical patient’s health information, and any interruption can literally mean life or death.
When you work to improve interoperability in healthcare, you’re operating in an environment where you can’t flip a switch and cut over to a new system. You need phased approaches, redundant systems, and detailed contingency plans for when things go wrong.
Poor communication during transitions contributes to over 60% of hospital adverse events. When information exchange breaks down between systems, the risk of miscommunication and information gaps rises dramatically. This puts patient safety at serious risk by increasing the chance of medical errors.
The connected healthcare ecosystem we’re building toward is absolutely worth pursuing, but getting there requires careful orchestration. Healthcare data must remain accessible, accurate, and timely throughout every phase of system modernization.
Healthcare organizations must carefully balance their interoperability initiatives to ensure patient safety never takes a backseat to technological progress. This means extended transition periods, parallel system operations, and extensive testing—all of which add time and cost to projects.
This is precisely why healthcare leaders increasingly turn to specialized interoperability solutions like Mediportal. Trying to overcome these challenges alone, with limited resources and competing priorities, is nearly impossible. The question isn’t whether investing in interoperability is worth it—it absolutely is. It’s about how to do it in a way that acknowledges these very real organizational, financial, and human constraints while moving forward.
Mediportal understands the significant challenges that healthcare organizations face across the United States. Our platform is designed to work within your constraints, providing phased implementation approaches that minimize disruption, reduce costs through efficient integration, and support interoperability without overwhelming your staff or compromising patient care.
Proven Strategies and Solutions for Overcoming Legacy System Barriers to Interoperability
You don’t have to be stuck with your legacy system forever. There are proven strategies to achieve interoperability without destroying your technology infrastructure. Healthcare organizations across the U.S. have successfully bridged the gap between old EMR systems and modern interoperability needs. They use smart, phased approaches that work with existing workflows.
Let’s explore the specific solutions that deliver results in real-world healthcare environments.
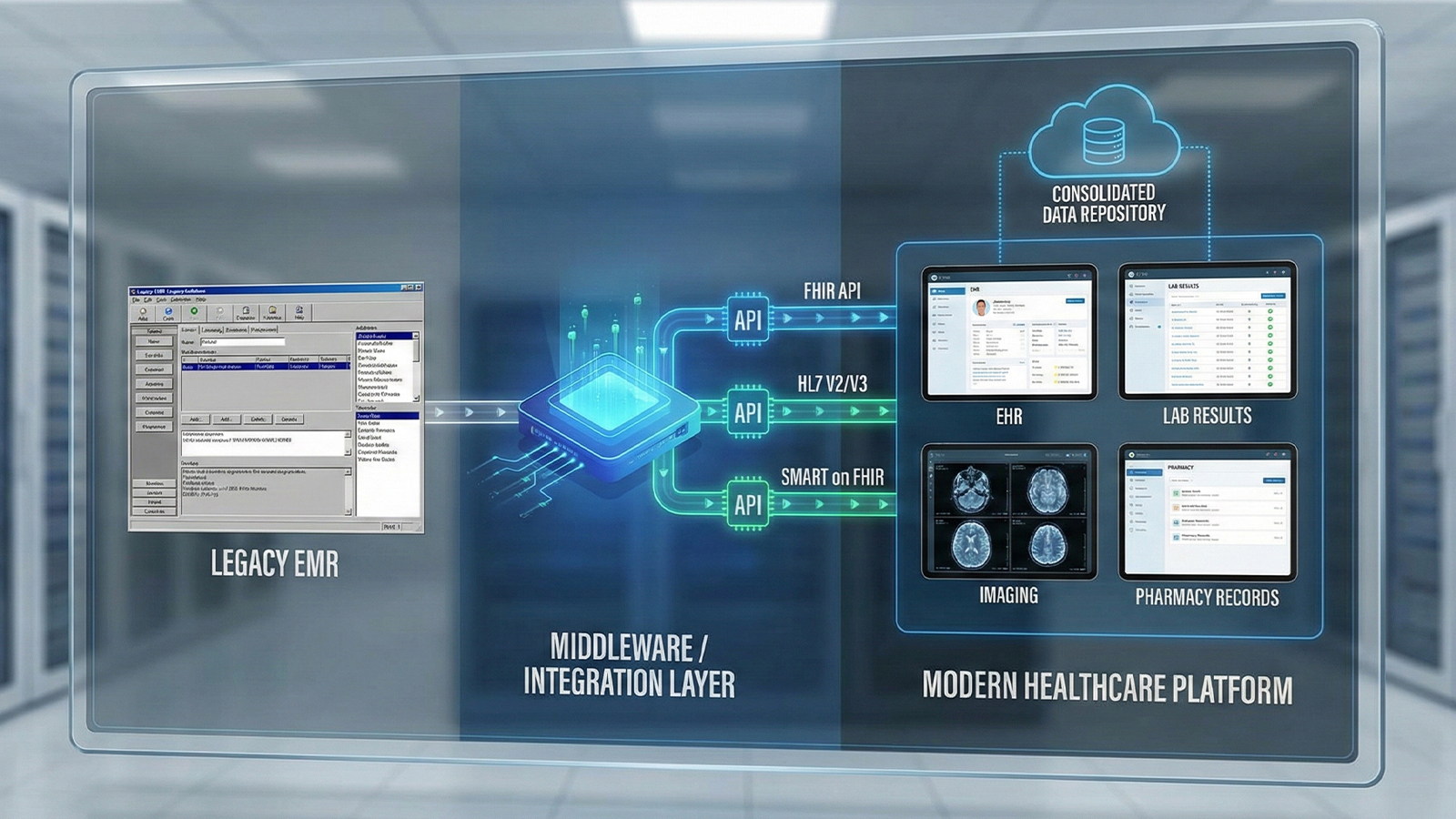
Implementing Healthcare Integration Platforms and Middleware Solutions
Middleware acts as the universal translator your legacy EMR needs. These integration platforms connect your outdated systems with modern applications. They enable seamless data exchange without requiring a complete system replacement.
APIs are the key to this connection. They allow disparate systems to communicate. Modern integration platforms use APIs that comply with standards like FHIR. This enables data exchange between legacy EMRs and contemporary healthcare applications.
Cloud-based integration platforms offer significant advantages. They can integrate with various data sources, ensuring interoperability across your healthcare ecosystem. These platforms provide robust security features and make information accessible when needed.
Some organizations are exploring blockchain technology for EHR interoperability. Blockchain creates a decentralized digital ledger for secure data exchange. This technology represents the cutting edge of secure data sharing.
Middleware approaches don’t require your legacy system to do something it wasn’t designed for. Instead, they create infrastructure that connects old and new systems. This maintains your existing workflows while building the connected ecosystem needed for interoperability.
Adopting Standardized Interoperability Frameworks
Investing in interoperability without embracing standardized frameworks is like building on sand. Interoperability frameworks like HL7 and FHIR provide a common language for healthcare data exchange. They ensure that everyone can understand the data being shared.
FHIR has emerged as the most promising standard for modern healthcare communication. Implementing solutions built on FHIR ensures that your systems can communicate with each other and external partners. APIs that comply with FHIR standards simplify interoperability by exchanging data in predictable formats.
The key is encouraging uniform adoption of standards like FHIR and HL7 across providers and regions. This creates compatibility with the broader healthcare ecosystem. When everyone speaks the same data language, compatibility issues disappear, and seamless data sharing becomes a reality.
Vendor selection is critical. Look for partners committed to open standards, not proprietary formats. Solutions that support interoperability frameworks like FHIR natively future-proof your investment. They adapt more easily as the healthcare industry evolves.
Steps to improve interoperability include adopting recognized standards, using clinical communications platforms built on these standards, and considering vendors’ open API frameworks. Establishing clear interoperability policies and investing in training ensures your team can leverage these standards effectively.
Phased Migration and Hybrid System Approaches
Most healthcare organizations can’t afford the downtime or financial hit of a “big bang” system replacement. Phased migration and hybrid approaches offer a solution.
Phased migration allows gradual transition, replacing or upgrading one component at a time. You might start by implementing a modern integration layer that connects to your legacy EMR. Then, gradually migrate specific departments or functions to newer systems as resources allow. This spreads costs over time and minimizes risk.
Hybrid approaches recognize the need to run legacy and modern systems side-by-side. They ensure data flows seamlessly between them. Consider these practical implementation strategies:
- Third-party archive solutions that preserve access to legacy data while transitioning to new systems
- Big data repositories that aggregate information from multiple sources into single accessible locations
- Consolidated clinical document architectures using standardized formats
- SMART on FHIR frameworks that allow modern applications to access legacy system data through standardized interfaces
The SMART on FHIR framework is worth special attention. It enables you to develop or implement modern applications that can access data from legacy systems. This creates a bridge between old and new technology, introducing new functionality without waiting for complete system replacement.
Phased approaches allow for learning and adjustment as you go. You can identify issues in early phases and correct course before they affect your entire organization. This iterative process reduces risk and improves outcomes compared to monolithic replacement projects.
How Mediportal Helps Healthcare Organizations Overcome These Challenges
Mediportal addresses these interoperability challenges with a practical approach. As a leading provider of healthcare interoperability software, we understand that you can’t just rip out legacy systems and start fresh.
Our platform is built on open standards including HL7 and FHIR. This ensures you’re investing in technology that will work with your current systems and future innovations alike. We provide the middleware and integration capabilities that allow your legacy EMR to communicate effectively with modern applications and other healthcare organizations.
Whether you’re a small community hospital or a large health system, Mediportal’s solutions meet you where you are. Our implementation approach emphasizes several key principles:
- Phased rollouts that maintain operational continuity throughout the transition
- Comprehensive training and support that addresses change management challenges head-on
- Ongoing optimization to ensure you’re getting maximum value from your interoperability investment
- Rapid ROI through improved efficiency, reduced duplicate testing, and better care coordination
We understand the financial constraints healthcare organizations face. Our solutions are designed to deliver measurable returns quickly. You’re not just spending money on technology—you’re investing in infrastructure that pays for itself through operational improvements.
But here’s what really makes the difference: specialized expertise. Most healthcare organizations don’t have integration specialists, clinical informaticists, and healthcare IT professionals who’ve successfully navigated these challenges dozens of times before. When you partner with Mediportal, you’re not just buying software—you’re gaining a team that’s genuinely invested in your success.
We’ve helped healthcare organizations across the United States transform their data exchange capabilities. They’ve improved patient outcomes and positioned themselves for success in an increasingly connected healthcare ecosystem. Our clients consistently report better care coordination, reduced administrative costs, and improved clinician satisfaction after implementing our interoperability solutions.
If you’re tired of wrestling with legacy system limitations and ready to move forward with interoperability solutions that actually work in the real world, that’s exactly what Mediportal delivers. We combine technical excellence with practical implementation strategies that acknowledge your operational realities and budget constraints while moving you steadily toward true interoperability.
Conclusion
Overcoming interoperability challenges with legacy EMR systems doesn’t mean you must replace everything at once. Healthcare organizations across the United States are successfully bridging the gap between outdated technology and modern data exchange needs. They do this without disrupting patient care.
Patient safety is the driving force behind interoperability improvements. When clinical teams have seamless access to complete information, they deliver better care. Effective system communication ensures your organization stays compliant, avoiding costly penalties or security risks.
Start by assessing your current interoperability gaps. Identify where data silos cause delays and which workflows frustrate your staff. Understanding these pain points helps you build a practical roadmap for improvement.
EHR transitions demand significant resources, but strategic planning reduces costs and disruption. Phased approaches, legacy data preservation, and specialized expertise make modernization manageable, even for budget-conscious healthcare providers.
Mediportal specializes in helping healthcare organizations navigate these challenges. Our interoperability solutions work with your existing infrastructure, creating bridges that deliver value quickly. They position you for long-term success.
You don’t have to solve these problems alone. The right partner understands your constraints and provides practical solutions that fit your reality. Ready to transform your approach to healthcare data exchange? Let’s discuss how Mediportal can help your organization achieve the connected, efficient care delivery system your patients and staff deserve.
FAQ
What is interoperability in healthcare?
Interoperability is the ability for different healthcare systems and applications to share, access, and use patient data seamlessly. It ensures clinicians have the right information at the right time, no matter where that data was created.
Why do legacy EMR systems struggle with interoperability?
Most legacy EMR systems were built before modern data standards like FHIR existed, so they weren’t designed to communicate easily with other platforms. As a result, they rely on outdated architectures, proprietary formats, or manual workarounds.
Can healthcare organizations improve interoperability without replacing their EMR?
Yes—many organizations use middleware or healthcare integration platforms to connect legacy systems with modern applications. This approach improves data exchange while avoiding the cost and disruption of a full system replacement.
How do interoperability challenges impact patient safety?
When systems can’t share data, clinicians may make decisions based on incomplete or delayed information. This increases the risk of medical errors, duplicate testing, and care coordination failures.
How does Mediportal help with legacy EMR interoperability?
Mediportal acts as a bridge between legacy EMR systems and modern healthcare technologies using standards like HL7 and FHIR. It enables secure, seamless data exchange without forcing organizations to abandon their existing infrastructure.